Embark on a journey into the world of Collaborating Physician Guide: How to Legally Partner in Telemedicine, where the intricacies of legal partnerships in telemedicine are unraveled in a captivating manner, offering a unique perspective on this evolving field.
Delve deeper into the nuances of collaborating physicians and their crucial role in shaping the landscape of telemedicine.
Overview of Collaborating Physician Guide in Telemedicine
Telemedicine involves providing healthcare services remotely using technology. Collaborating physicians in telemedicine work together to deliver quality care to patients, leveraging each other's expertise and resources. Legal partnerships are crucial in telemedicine to ensure compliance with regulations and provide a seamless patient experience.
Importance of Legally Partnering in Telemedicine
Legal partnerships in telemedicine help physicians navigate complex healthcare laws and regulations. By partnering with other healthcare professionals, physicians can expand their reach, offer specialized services, and ensure patient safety. Compliance with state and federal laws is essential to protect both patients and providers.
Examples of Collaborating Physicians in Telemedicine
- Primary care physician partnering with a specialist to provide comprehensive care to patients.
- Psychiatrist collaborating with a therapist to offer mental health services remotely.
- Tele-radiology group working with local hospitals to provide timely diagnostic imaging interpretations.
Legal Requirements for Collaborating Physicians
When it comes to collaborating in telemedicine, physicians must adhere to specific legal requirements to ensure compliance and quality care delivery. This includes licensing, credentialing, and considerations for liability and malpractice.
Licensing and Credentialing Process
- Physicians must hold a valid license in the state where the patient is located during the telemedicine consultation.
- Credentialing processes may vary among healthcare organizations, but collaborating physicians must meet specific qualifications and standards to participate in telemedicine programs.
- Verification of qualifications, experience, and training is essential to ensure that collaborating physicians are competent to provide care remotely.
Liability and Malpractice Considerations
- Collaborating physicians should have clear agreements outlining their roles, responsibilities, and liability coverage when providing telemedicine services.
- Understanding the legal framework for telemedicine practice is crucial to mitigate risks and ensure patient safety.
- Proper documentation of telemedicine consultations and adherence to state laws and regulations can help protect collaborating physicians from malpractice claims.
Establishing a Collaborative Agreement
In order to legally partner in telemedicine, it is crucial to have a well-defined collaborative agreement in place. This agreement Artikels the responsibilities of both the collaborating physician and the telemedicine provider, ensuring that all legal and ethical guidelines are followed throughout the partnership.
Steps to Create a Collaborative Agreement
Creating a collaborative agreement involves several key steps to ensure that both parties are on the same page and that all legal requirements are met. Here is a general framework for establishing a legally binding collaborative agreement in telemedicine:
- Identify the parties involved: Clearly state the names and contact information of the collaborating physician and the telemedicine provider.
- Define the scope of practice: Artikel the specific services that the collaborating physician will provide in the telemedicine setting.
- Establish communication protocols: Detail how the collaborating physician will communicate with the telemedicine provider, including frequency and methods of communication.
- Set terms for patient care: Define how patient care responsibilities will be divided between the collaborating physician and the telemedicine provider.
- Include termination clauses: Artikel the circumstances under which the agreement can be terminated by either party and the process for doing so.
Key Components of a Collaborative Agreement
A legally binding collaborative agreement in telemedicine should include the following key components to ensure clarity and compliance with legal and ethical standards:
- Names and contact information of the parties involved
- Scope of practice for the collaborating physician
- Details on communication protocols
- Terms for patient care and responsibilities
- Termination clauses and procedures
- Compliance with state and federal telemedicine regulations
Maintaining Compliance in Telemedicine Collaboration
Maintaining compliance in telemedicine collaboration is crucial to ensure that all activities are conducted within legal boundaries and patient safety is prioritized. Collaborating physicians must adhere to telemedicine regulations, maintain patient confidentiality, and secure data to uphold compliance standards.
Importance of Patient Confidentiality and Data Security
Ensuring patient confidentiality and data security is paramount in telemedicine collaboration to protect sensitive information and maintain trust with patients. Collaborating physicians must implement secure communication channels, encryption technologies, and access controls to safeguard patient data from unauthorized access.
Best Practices for Compliance
- Regularly review and update collaborative agreements to reflect current regulations and standards.
- Provide comprehensive training to all staff members on telemedicine compliance protocols and data security measures.
- Implement secure telemedicine platforms that comply with HIPAA regulations for safeguarding patient information.
- Conduct regular audits and assessments to identify any compliance gaps and address them promptly.
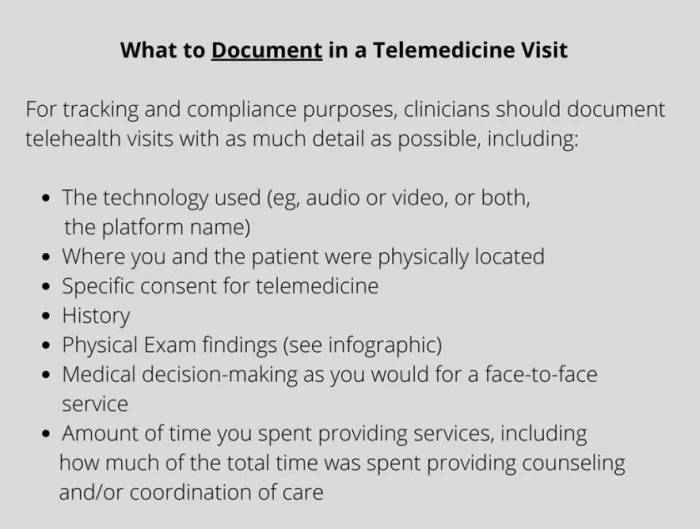
- Maintain detailed documentation of all telemedicine interactions and communications for compliance purposes.
Last Word
As we reach the conclusion of this exploration, a comprehensive summary of the key aspects covered sheds light on the essential principles of legally partnering in telemedicine, leaving a lasting impression on readers.
FAQ
What legal requirements do physicians need to collaborate in telemedicine?
Physicians collaborating in telemedicine must ensure compliance with state licensing laws and credentialing requirements specific to telehealth practice.
How can collaborating physicians maintain patient confidentiality in telemedicine?
Collaborating physicians can uphold patient confidentiality by using secure communication channels, encrypting data, and following HIPAA guidelines.
What are some best practices for collaborating physicians to stay compliant in telemedicine?
Best practices include regular training on telemedicine regulations, conducting thorough risk assessments, and implementing robust data security measures.






![Trulicity Eye Side Effects Lawsuit [2025 Update] | King Law](https://medic.goodstats.id/wp-content/uploads/2025/12/Trulicity-Side-Effects-Common-Serious-Long-term-1-120x86.png)



